What are the Symptoms of Mold Toxicity?
Article at a Glance
Mold exposure can lead to a wide array of health issues—from allergic reactions and chronic inflammation to more severe problems such as autoimmune disease, cognitive impairments, and even cancer.
This guide offers an in-depth look at the myriad of symptoms caused by mold toxicity as well as:
- The mechanisms of damage
- Who is most susceptible
- How to get a diagnosis
- The best approaches for treatment.
- Frequently Asked Questions (FAQ’s)
What are the symptoms of mold toxicity? Let’s dive in and take a deeper look.
table of contents
Introduction: Why Mold Matters
Understanding Mold and Mycotoxins
Mechanisms of Mold and Mycotoxin-Induced Damage
Why Are Some People More Affected By Mold Than Others?
Diseases Linked to Mold and Water-Damaged Buildings
Mold, Mycotoxins, and Cancer: An Evolving Discussion
Why Mold Matters
Mold thrives in damp, humid conditions. It is commonly found in water-damaged buildings, and according to the National Institute for Occupational Safety and Health (NIOSH), almost 50% of buildings in the US are water damaged. This amasses to a health crisis of epidemic proportions.
Mold produces spores, mycotoxins, volatile organic compounds (VOCs), and hyphal fragments capable of causing a host of health issues ranging from mild allergic reactions to severe chronic inflammatory diseases. For example, mycotoxins have been linked to cancers, and nerve damage. Mold infections (mycoses) can lead to the formation of fungal balls (masses) in the body. These masses can look tike tumors, and can lead to misdiagnosis and improper treatment.
While many are aware of mold-induced respiratory problems, fewer recognize the full spectrum of symptoms, syndromes, and diseases that mold can cause or contribute to.
Understanding Mold and Mycotoxins
What is Mold?
According to the National Institute of Environmental Health Sciences:
Mold is a microorganism and type of fungus that thrives in wet places. In nature, it forms on damp materials and in decaying organic matter. Outdoor mold reaches its highest levels in the summer and fall. Inside, it can spread on damp surfaces, like the paper surface of wet drywall. Flooding, leaky pipes, humid conditions, and poor ventilation contribute to the growth of mold in our buildings and homes.
Simply put, mold is God’s great recycler. Mold’s purpose in nature is to break down dead organic matter and recycle nutrients back into the environment. Stachybotrys chartarum, Aspergillus, Penicillium, Fusarium, Chaetomium, and Cladosporium are common molds found at higher levels in damp or water damaged buildings. These molds can produce toxic compounds referred to as mycotoxins.
What are Mycotoxins?
Myco = Mold. Mycotoxins are as the name implies…toxic compounds produced by mold. These toxins are capable of causing disease and death in both humans and other animals. They are commonly found in contaminated food crops like grains. They are also commonly found in water damaged buildings. They can be absorbed through the skin, the lungs, and the GI tract. When someone develops illness from mycotoxin exposure, it is referred to as mycotoxicosis.
Common Types of Indoor Mold & the Mycotoxins They Produce
- Stachybotrys chartarum: Often referred to as black mold or “Stachy”. Stachy produces a group of mycotoxins called trichothecenes. These toxins are linked to immunosuppression, nerve, and vascular damage.
- Aspergillus species: Produces aflatoxins, implicated in liver cancer.
- Penicillium species: Rapidly colonizes damp materials, releases various mycotoxins including ochratoxin A (OTA). OTA has been linked to cancer and kidney disease.
- Fusarium: Colonizes damp materials and produces fumonisin and an estrogen mimicking toxin called Zearalenone (Zea)
- Chaetomium: Produces several mycotoxins linked to brain and liver damage as well as cancer.
- Cladosporium species: Common in HVAC systems; triggers allergies and asthma.
Mold & Mycotoxin-Induced Damage
Below is a simple breakdown of the 5 major ways mold and it’s toxins can contribute to health problems.
- You can be allergic to mold spores. It is estimated that 22% of the population has an allergy to at least one type of mold.
- You can have an immune response to mold & mycotoxins. This is sometimes referred to as a hypersensitivity.
- You can have inflammatory reactions to mycotoxin exposure that cause or contribute to diseases. This is referred to as mycotoxicosis.
- You can develop a mold infection. This is referred to as mycoses. This typically occurs in people with suppressed immune systems. For example, people with cancer or HIV have compromised immunity. Additionally, many medications cause immune suppression. Examples include, steroids, biologics, allergy medications, covid \/accinations, and chemotherapy.
- Beyond mold and mycotoxins, you can have inflammatory reactions to mold fragments and VOC’s (Volatile Organic Compounds) produced by mold.
How Mold & Mycotoxins Cause Damage (For the Advanced Reader)
Inhibition of DNA, RNA, and Protein Synthesis
Several mycotoxins (e.g., trichothecenes and aflatoxins) disrupt ribosomal function, preventing cells from synthesizing protein, RNA, and DNA. This inhibition contributes to tissue damage, inhibition of healing, and cell death.
Let’s translate that into something more understandable. When mycotoxins block DNA, RNA, and protein production in humans, our body goes into a repair deficit state. Many with chronic mycotoxin exposure describe their experiences as accelerated aging. They feel like their bodies breaking down faster and healing slower.
Oxidative Stress and Inflammatory Pathways
Mycotoxins such as ochratoxin A, aflatoxin, trichothecenes, and ZEA generate reactive oxygen species (ROS), causing cellular damage, mitochondrial dysfunction, and chronic inflammation. In case you are wondering, an ROS is a free radical, or unstable molecule capable of causing tremendous damage to our bodies.
Neurotoxicity
Some mycotoxins cross the blood-brain barrier and damage nerve cells. Some research has demonstrated brain damage visually by using an MRI technology called Neuroquant®.
Endocrine Disruption
Some mycotoxins have been shown to contribute to liver and pancreatic metabolic issues. Some mycotoxins that mimic estrogen have been linked to cancers and fertility issues.
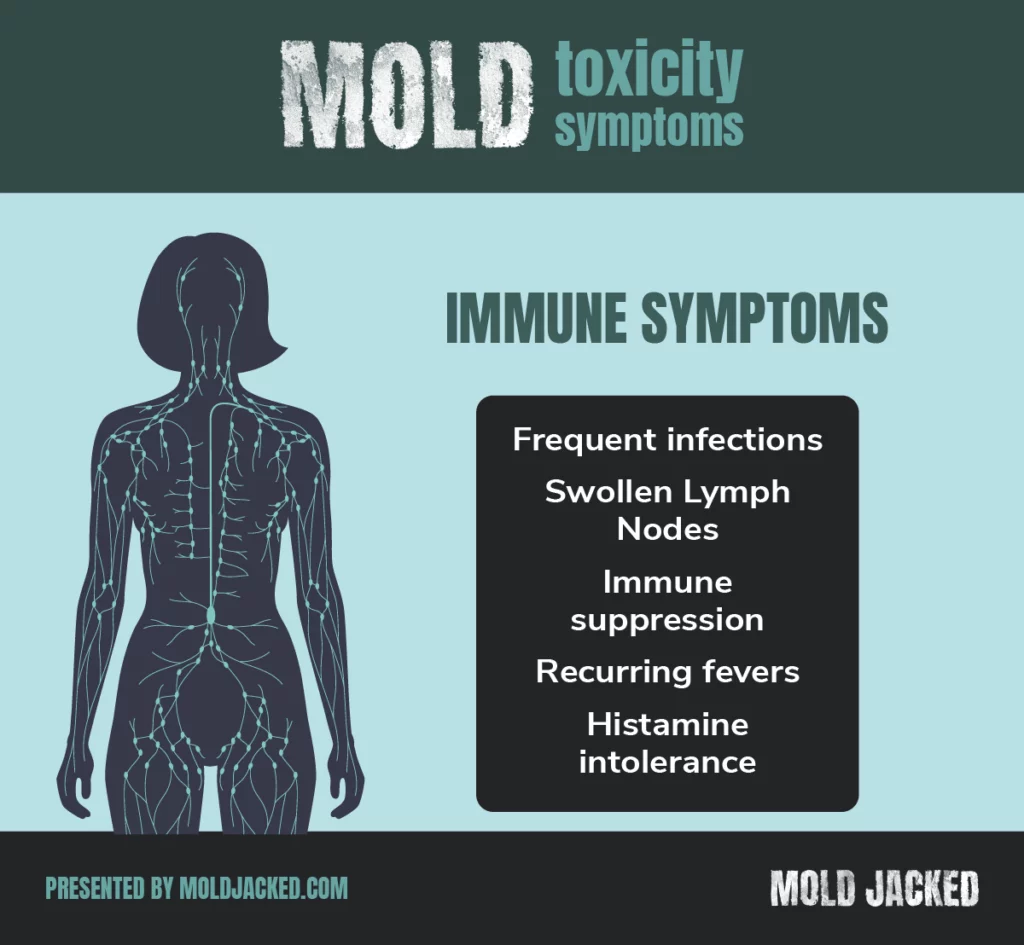
Immune Modulation
Mycotoxins have been shown to cause both immune suppression and over-activation. These can predispose to infection and autoimmune disease respectively.
Why Are Some People More Affected By Mold Than Others?
When it comes to mold, not everyone is affected the same. There are a variety of factors that can play a role in susceptibility and severity of mold related illness.
- Age – Infants, children, and elderly are at greater risk
- Size – In my experience, smaller women and children are typically impacted before others in the home. Sometimes, the mysterious death of small pets can be the first warning of mold toxicity in an environment.
- Time and dose of exposure
- Acute Exposure: High-level, short-term contact often triggers immediate, severe symptoms (e.g., coughing fits, skin rashes).
- Chronic Exposure: Low-level, long-term contact (e.g., living in a damp home) leads to gradual yet persistent issues, from mild respiratory irritations to severe systemic inflammation. Chronic exposure is much more challenging to diagnose. When the home is the source of mold exposure, stay at home moms and children often develop more symptoms.
- Location of the mold – Sometimes mold is a systemic problem throughout the home. Sometimes mold growth is isolated to certain areas of a home, making some family members more sick than others.
- Genetics – Some research has identified that certain HLA DR genotypes increase the risk for susceptibility of mold related illness. Additionally, some people have genetic variants for detoxification that may impact their ability to metabolize and clear mold toxins.
- Poor Lifestyle Habits – Consumption of processed foods, smoking, excessive alcohol, inadequate sleep, inadequate sun exposure, lack of physical activity, & fluoridated water consumption can create immune dysfunction and increase susceptibility to mold related illness.
- Mold Heavy Diets – Grains, dried fruits, peanuts, chocolate, grain fed animal meats and dairy, and alcohol are commonly contaminated with mycotoxins.
- Nutritional Deficiencies – Vitamins, minerals, and other nutrients are required for protecting the body, supporting detoxification, maintaining metabolism, and promoting healing. Mold exposure increases the body’s need for these nutrients, which are essential for these functions. If someone already has nutritional deficiencies, mold-related illness may be exacerbated. Some research suggests that mold exposure can contribute to vitamin B12 deficiency. Additionally, mold toxins can damage the gut, leading to malabsorption, which may further increase the risk of nutrient deficiencies.
- Work Related Risks – According to researchers, an estimated 50% of buildings are water damaged. Aging infrastructure and inadequate maintenance related to moisture control are common problems. During Covid, the lockdowns left buildings unoccupied. In many of these buildings, air conditioning was either reduced or discontinued to save money. Reports show that this has led to a major building mold infestations as well as microbial contamination in building water systems. In my clinical experience, I have seen hundreds of patients be exposed to mold in their work environments. In one case, a teacher had recurring health issues at the beginning of every school year. She would go into remission during the Summer. The school was eventually torn down because of severe mold infestation. Other professions are at risk for mold related illness include musicians playing wind instruments, farmers, and wood workers.
- Risks Outside of the Home & Workplace – Mold exposure is not limited to residential or occupational settings; it can also occur in various environments such as schools, gyms, vehicles, and public buildings. Those spending inordinate amounts of time in contaminated locations increase their overall exposure and risk of illness.
- Pre-Existing Illnesses – Those with pre-existing chronic inflammatory diseases are more susceptible to mold.
- History of Chronic Antibiotic Use – Antibiotics have been linked to increased risk of life threatening yeast infections. Yeast can produce fungal toxins that are similar to mold toxins leading to immune suppression.
- Medications – As mentioned above, medicines that affect the immune system increase risk of mold infection.
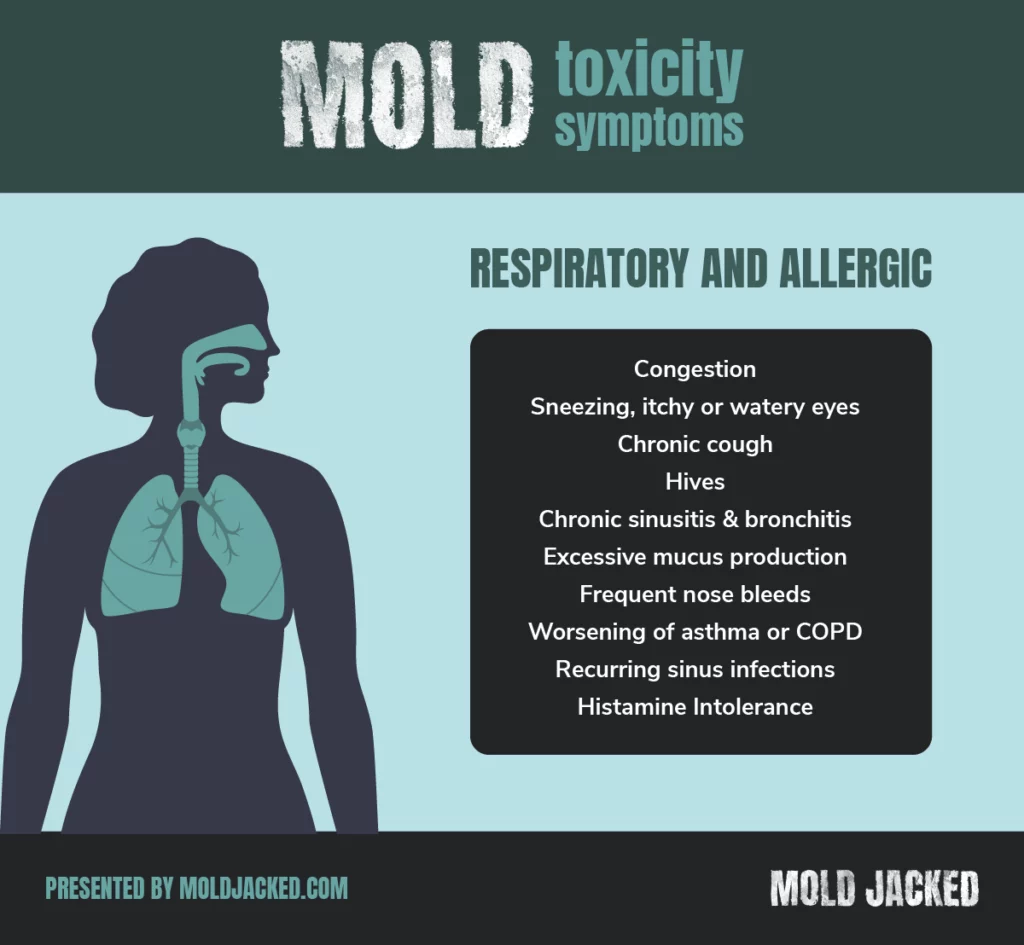
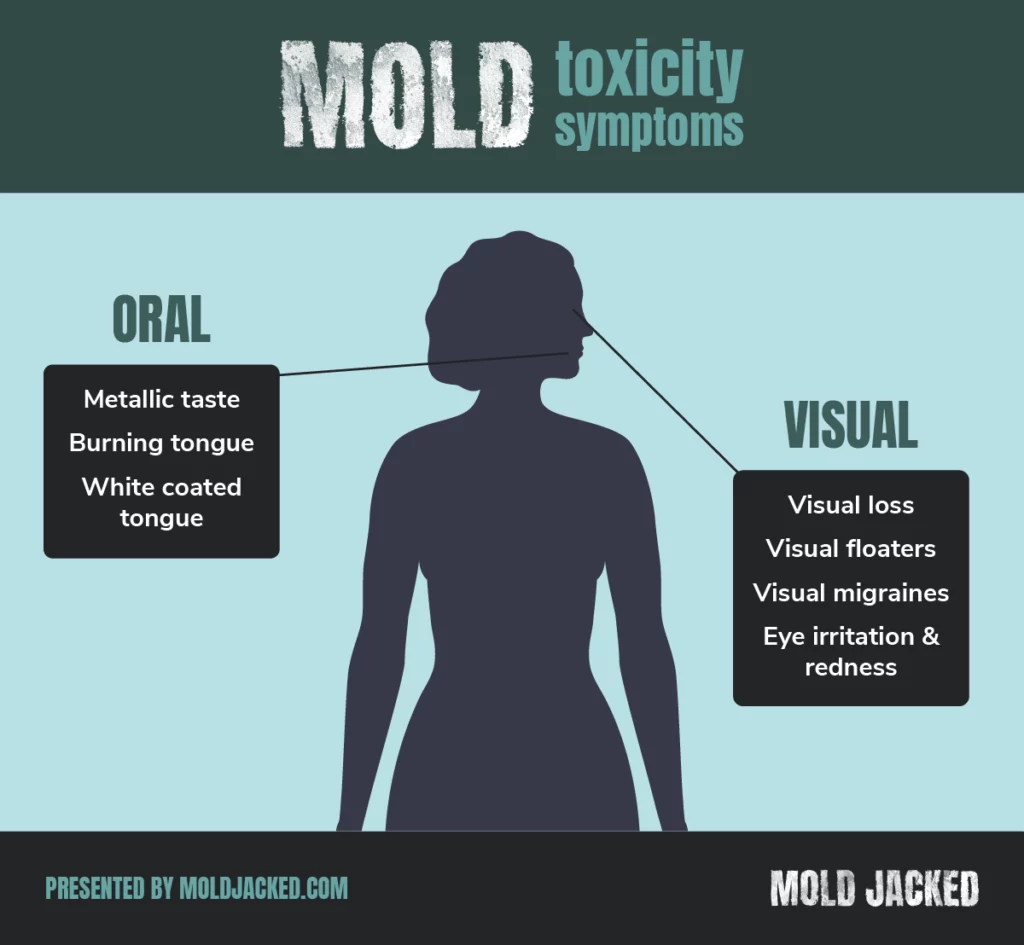
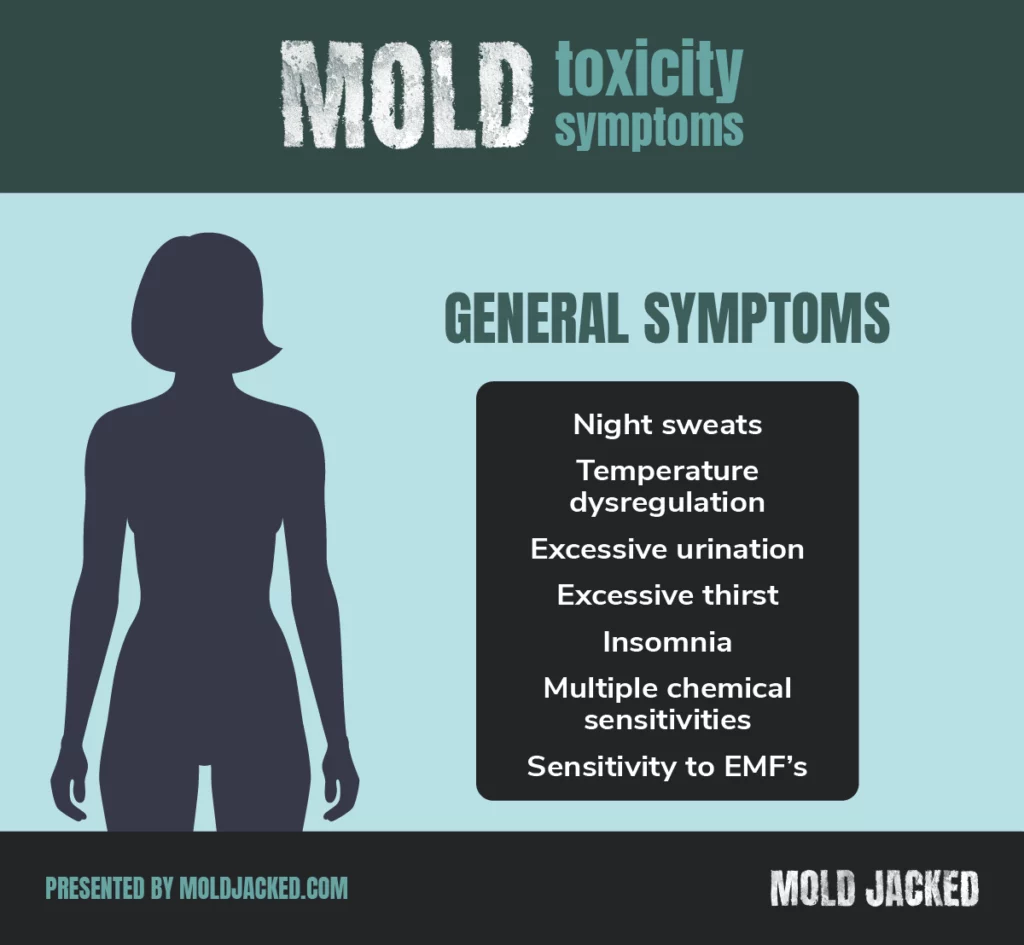
What are the symptoms of mold toxicity?
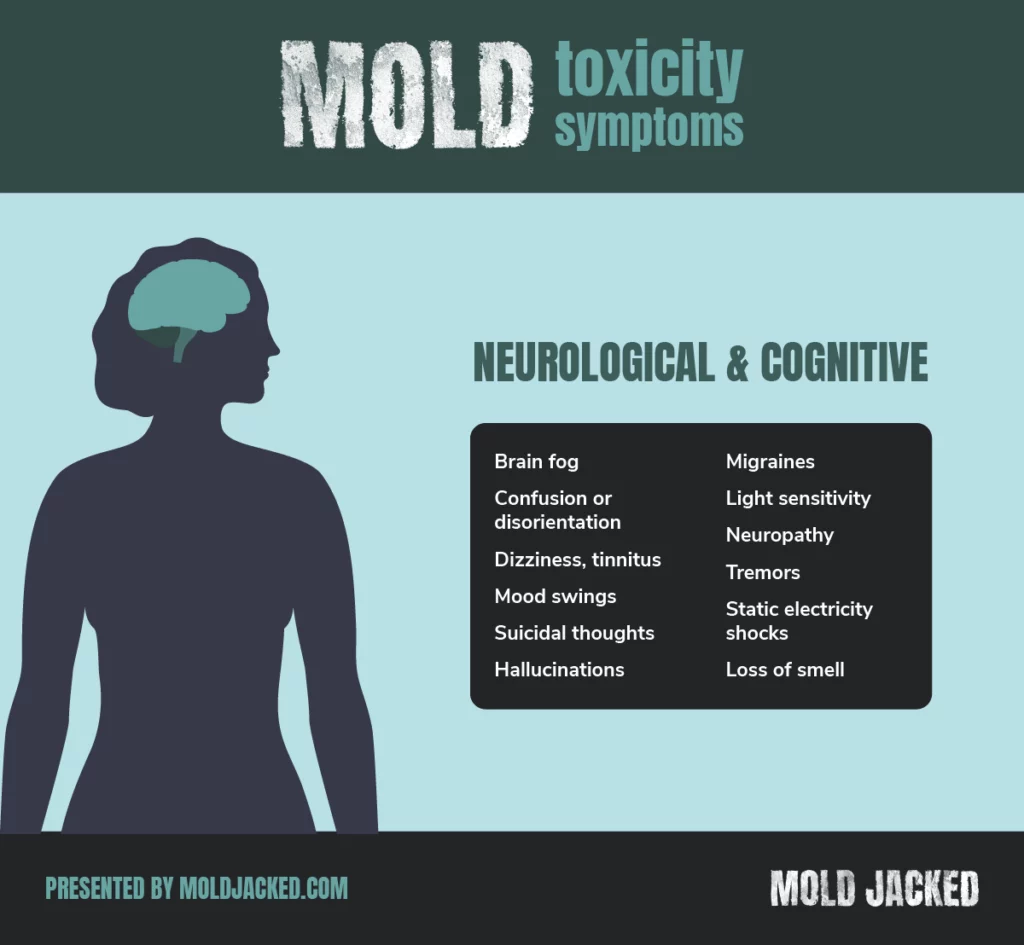
Neurological and Cognitive Symptoms
- Brain fog, impaired concentration, inability to learn, remember, or recall words
- Confusion or disorientation
- Dizziness, tinnitus
- Mood disturbances (anxiety, depression, mood swings)
- Suicidal ideations
- Hallucinations
- Migraine headaches
- Light sensitivity
- Neuropathy – burning, numbness, or tingling
- Tremors
- Static electricity shocks
- Loss of smell
Common Lab Abnormalities
The following are lab tests commonly run by doctors during annual check ups. If you have a history of the following test abnormalities coupled with the symptoms above, you should talk with your doctor about toxic mold.
- Low white blood cells (WBC), red blood cells (RBC), and platelets
- Elevated liver markers (AST, ALT, Bilirubin)
- Elevated ferritin
- Low eGFR
Diseases Linked to Toxic Mold Exposure
Now that you have a deeper understanding of what symptoms are caused by mold toxicity, let’s dive into some diseases that can develop or be exacerbated by toxic molds.
Allergic Diseases
- Rhinitis and sinusitis
- Asthma
- Chronic Obstructive Pulmonary Disease (COPD)
- Mast Cell Activation Syndrome (MCAS)
Diseases of Chronic Immune Disruption
A growing body of evidence has linked various autoimmune and other related illnesses to mold and mycotoxin exposures. Research shows that whether mycotoxins are eaten or inhaled, they gain systemic access to the rest of the body. This allows them to travel to any tissue in the body causing immune dysfunction and inflammation.
- Hypersensitivity Pneumonitis (Mold-Induced Lung Inflammation)
- Autoimmune Disease – Mold toxins can cause intestinal hyperpermeability (Leaky Gut), a common trigger for autoimmunity.
- Multiple Sclerosis
- Neuropathy
- Rheumatoid Arthritis
- Colitis
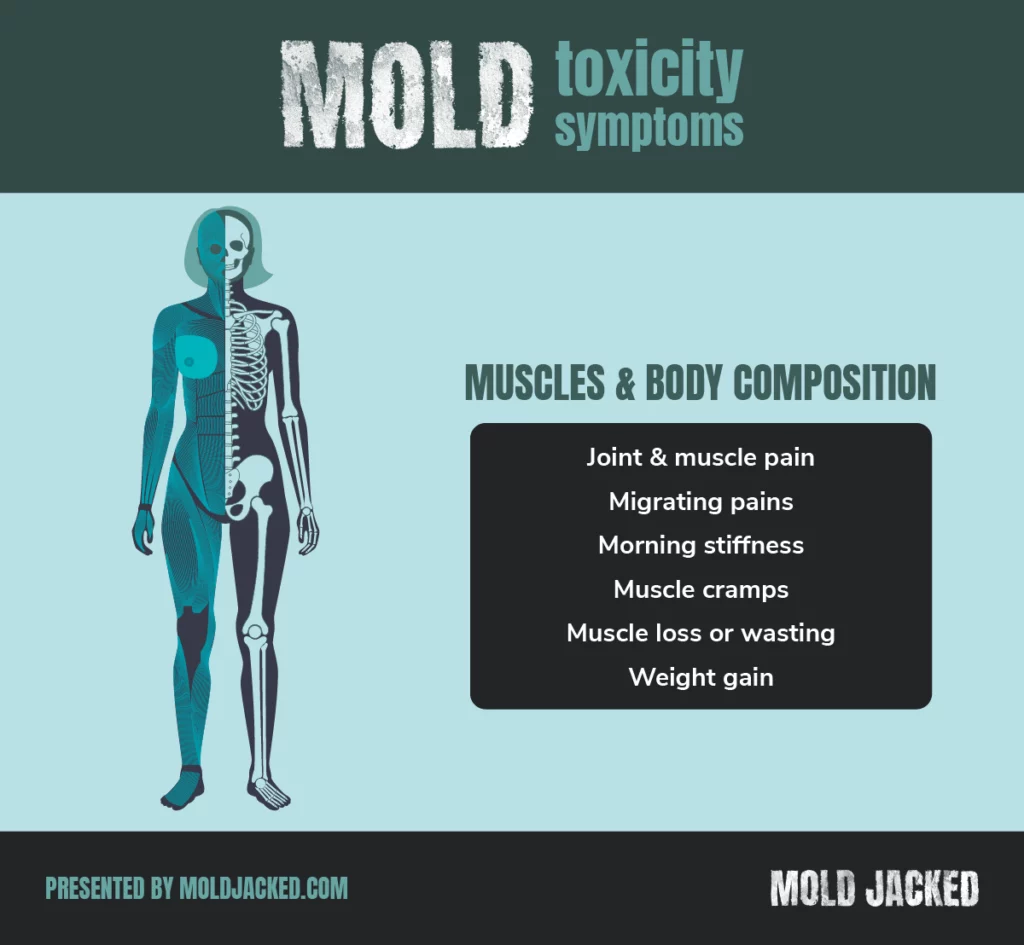
- Fibromyalgia
- Chronic Fatigue Syndrome (CFS)
- Myalgic Encaphalitis (ME)
- PANS/PANDAS
- Autism
Chronic Inflammatory Response Syndrome (CIRS)
A leading medical authority on mold illness, Dr. Ritchie Shoemaker, is responsible for defining CIRS.
Chronic Inflammatory Response Syndrome (CIRS) is an acquired medical condition characterized by innate immune dysregulation following respiratory exposure to water-damaged buildings (WDB). This chronic syndrome involves a range of symptoms that simultaneously affecting multiple organ systems.
In his research, Dr. Shoemaker has shown that mold, bacteria, and the toxins they produce are responsible for triggering immune inflammation leading to the symptoms that people experience in water damaged buildings.
Sick Building Syndrome (SBS)
SBS is also sometimes referred to as Tight Building Syndrome (TBS). According to the EPA,
The sick building syndrome (SBS) is used to describe a situation in which the occupants of a building experience acute health- or comfort-related effects that seem to be linked directly to the time spent in the building. No specific illness or cause can be identified. The complainants may be localized in a particular room or zone or may be widespread throughout the building.
Common symptoms include headache, dizziness, nausea, eye, nose or throat irritation, dry cough, dry or itching skin, difficulty in concentration, fatigue, sensitivity to odors, hoarseness of voice, allergies, flu-like symptoms, increased incidence of asthma attacks and personality changes.
Infectious Mold Disease (Mycoses)
Under the right circumstances, mold can colonize and infect humans. Over the past several decades, this problem has been increasing. The World Health Organization recently published a report on this growing threat.
Emerging from the shadows of the bacterial antimicrobial resistance pandemic, fungal infections are growing, and are ever more resistant to treatments, becoming a public health concern worldwide. – Dr Hanan Balkhy, WHO Assistant Director-General, Antimicrobial Resistance (AMR)
Mold infections can be present on the skin, the sinuses, the GI tract, lungs, the eyes, nervous system, the brain, in the bones and in joints. Mold infections can also be systemic. Typically, those at risk for mold infections are immune compromised. Patients being treated with immune suppressing medications can be targets of mold infection. Those living in mold contaminated buildings, cancer patients, and HIV patients are also considered immune compromised.
Respiratory and Sinus Infections
- Allergic Bronchopulmonary Aspergillosis (ABPA) – An allergic reaction to Aspergillus mold in the lungs, leading to wheezing, shortness of breath, and lung damage over time.
- Chronic Pulmonary Aspergillosis (CPA) – A long-term lung infection caused by Aspergillus that can lead to cavities (holes) in the lungs.
- Fungal Rhinosinusitis (Chronic and Acute) – Sinus infection caused by molds like Aspergillus, Mucor, or Alternaria, leading to nasal congestion, headaches, and facial pain.
- Hypersensitivity Pneumonitis (Mold-Induced Lung Inflammation) – An immune reaction to mold spores in the lungs, causing coughing, shortness of breath, and flu-like symptoms.
- Aspergilloma (Fungal Ball) – A mass of Aspergillus mold growing in pre-existing lung cavities, often in people with tuberculosis or COPD.
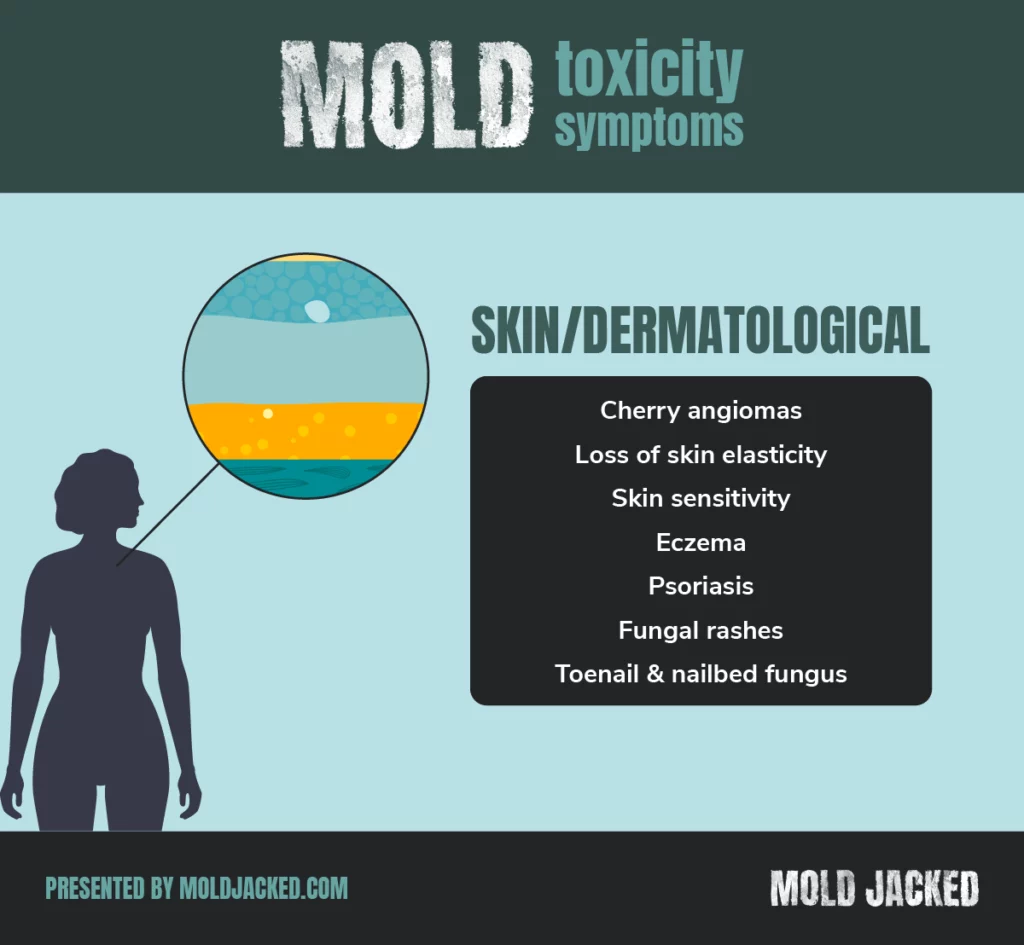
Skin and Soft Tissue Infections
- Subcutaneous Mucormycosis – Mucor or Rhizopus fungi infect wounds, leading to deep tissue damage.
- Tinea (Ringworm, Athlete’s Foot, Jock Itch) – Fungal infections of the skin, caused by molds like Trichophyton, Microsporum, and Epidermophyton.
- Chromoblastomycosis – A slow-spreading skin infection caused by black molds (Fonsecaea, Phialophora), often from soil contact.
- Eumycetoma (Madura Foot) – Chronic deep fungal infection affecting the skin, muscles, and bones, caused by Madurella species.
Invasive and Systemic Fungal Infections
- Invasive Aspergillosis – A life-threatening infection where Aspergillus spreads from the lungs to the brain, heart, kidneys, and other organs, mostly in immunocompromised people.
- Disseminated Histoplasmosis – Severe, body-wide infection caused by Histoplasma capsulatum, spreading from the lungs to the liver, spleen, and bones.
- Paracoccidioidomycosis (South American Blastomycosis) – Caused by Paracoccidioides species, affecting the lungs, skin, and mucous membranes.
- Talaromycosis (Penicilliosis Marneffei) – A systemic infection caused by Talaromyces marneffei (formerly Penicillium marneffei), common in HIV/AIDS patients in Southeast Asia.
- Candidiasis (Systemic or Mucosal) – While mostly caused by Candida yeast, systemic infections can sometimes involve mold-like fungi in immunocompromised patients.
Eye Infections
- Fungal Keratitis – An eye infection caused by Fusarium, Aspergillus, or Candida, often after trauma or contact lens use, leading to vision loss if untreated.
- Endophthalmitis – A severe, sight-threatening fungal infection inside the eye, sometimes caused by Aspergillus or Candida in immunocompromised people.
Neurological Infections
- Cryptococcal Meningitis – Caused by Cryptococcus neoformans, a mold-like fungus found in soil and bird droppings, leading to brain infections, especially in immunocompromised people.
- Cerebral Aspergillosis – Aspergillus spreads to the brain, causing severe neurological symptoms like seizures, confusion, and coma.
Gastrointestinal Fungal Infections
- Gastrointestinal Mucormycosis – A rare but severe infection affecting the stomach or intestines, often seen in people with weak immune systems.
- Histoplasmosis Gastrointestinal Involvement – In rare cases, Histoplasma infection can affect the digestive tract, leading to ulcers and intestinal blockage.
- Candidiasis – a yeast that has been linked to inflammation and cancers.
Bone and Joint Infections
- Fungal Osteomyelitis – Bone infection caused by Aspergillus, Blastomyces, or Coccidioides, leading to chronic pain and bone damage.
- Septic Arthritis (Fungal Joint Infection) – Candida, Aspergillus, or Sporothrix species can infect the joints, causing pain, swelling, and stiffness.
Mold, Mycotoxins, and Cancer: An Evolving Discussion
Fungal Infections that Mimic Tumors
Numerous medical studies and case reports have shown that certain mold infections can be mistaken for different types of cancer. For example, mucormycosis or invasive aspergillosis can form fungal masses, especially in the brain or lungs. These masses appear tumor-like on imaging scans, contributing to the possibility of a misdiagnosis. Fungal infections of the skin can also be misdiagnosed as cancers.
Fungal DNA Found in Tumors
The infectious theory of cancer has strong research supporting the fact that microbial infections can cause, contribute to or exacerbate cancer growth. Recent evidence has emerged where scientists have identified fungal DNA in tumors of the head-neck, breast, lung, stomach, skin, and colon. Some researchers speculate that this may speed up the rate of cancer growth.
It is not clear yet whether mold is causal in these cancers, but several research studies have linked the use of anti fungal medications to improved cancer outcomes. In addition, a growing number of people are turning to drugs like ivermectin and fenbendazole to treat their cancers. The anecdotal outcomes have been positive for many.
Mycotoxins: Potential to Cause Cancer
Certain mycotoxins have been linked to cancer development. According to the International Agency for Research on Cancer (IARC) the following mycotoxins are classified as carcinogens:
- Aflatoxins – Classified as a group 1 carcinogen. Group 1 means a definitely cancerous to humans.
- Fumonisin – Classified as a group 2b carcinogen. Group 2b means possibly carcinogenic to humans.
- Ochratoxin A – Classified as a group 2b carcinogen.
- Many other mycotoxins have been show to cause tumors in animal studies, but inadequate human studies exist. The biological mechanisms of how mycotoxins create damage have been elucidated in many studies. These mechanisms are known to contribute to the development of cancer.
Assessment for Mold Toxicity
It is important to work with a mold literate doctor when seeking professional guidance. This is not an area or research that is taught in medical school. Mold literate doctors typically take post graduate training to gain additional knowledge and understanding. When interviewing doctors, a simple question that can be asked is: “Do you perform laboratory testing to help identify mold and mycotoxin exposures?” Below are some simple expectations that you should have when being assessed by a doctor.
Clinical Evaluation
A doctor should perform the following to help determine whether or not mold may be contributing to your illness:
- Exposure History: Home/work environment, history of water intrusion or damage, musty smells, regional climate, and additional questions to help assess the likelihood of exposure.
- Symptom Review: Multi-system assessments (respiratory, neurological, musculoskeletal, gastrointestinal, dermatological, etc).
- Physical Exam: Signs of mold related illness can leave physical clues. Skin changes, muscle and joint problems, neuropathy, and many other issues can be assessed in a physical examination.
Laboratory Tests
The following lab tests are commonly used to assess for mold and mycotoxin related illness. This list is not exhaustive, and a mold literate doctor may want to recommend additional testing:
- Mycotoxin Panels: Urine tests for trichothecenes, aflatoxins, ochratoxin A, and other mold toxins.
- Antibody Levels: Antibodies to assess for immune reactions against mold and mycotoxins can be helpful.
- Inflammatory Markers: CRP, TGF-β1, MMP-9, C4a, ferritin, cytokine panels.
- HLA Typing: Genetic predisposition checks (e.g., for CIRS)
- NeuroQuant MRI – Some clinicians use advanced MRI techniques to detect brain volumetric changes consistent with mold toxin-related illnesses (e.g., CIRS).
Environmental Testing
A mold literate doctor may refer you to an inspector to investigate the following:
- Air & Dust Sampling: Compare indoor vs. outdoor spore counts.
- PCR Analysis: ERMI/HERTSMI-2 to detect mold DNA.
- Professional Inspection: Certified mold inspectors or building biologists can find hidden sources (wall cavities, crawlspaces, HVAC).
Treatment and Management of Mold Toxicity
Ultimately, you should follow the advice of your doctor. Mold treatment and management can be a challenging endeavor. Make sure that you avoid the #1 mistake people make. What is it? They stay in their moldy environment. Recovering from mold and mycotoxin related illness requires a safe and clean environment. Your doctor should walk you through an objective process to help you accomplish this. As a general rule, the following items should all be considered as essential to a holistic approach to recovery.
Environmental Remediation
The two most important aspects to a successful remediation are – 1. Find the source of the mold, and 2. Identify the source of moisture that allowed it to grow. Once you know the answer to both, a successful remediation can be planned. A competent mold inspector can help you determine this. If you haven’t already, read our guide on how to hire a mold inspector here.
Remediation typically consists 4 basic steps:
- Quarantine the contaminated area – a remediation company should seal off the rest of the home with containment walls to prevent cross contaminating mold free areas.
- Remove mold contaminated materials – all moldy materials should be removed from the home.
- Clean Up – The use of air scrubbers, HEPA vacuums, and microfiber cloths to wipe down walls, ceilings, floors and solid items in the home. If necessary, fine particle remediation should also be performed.
- Evaluate the success of the job – Have an independent mold inspector come back to the home after remediation is complete to assess whether the job was performed successfully. **Don’t skip this step. When successful, your home should receive a mold clearance certificate as proof of success. You may need this later should you sell the home.
For more details, please read our Mold Remediation Guide.
Medical Treatments & Nutritional Support Options
Now that you are in a safe environment, the real work can begin. Depending on your doctors assessment, several types of treatment and nutritional support options may be recommended. Some common ones include:
- Binders & Detox Aids: Activated charcoal, zeolite, bentonite clay, or other over the counter binders may be recommended by your doctor. Some doctors also recommend the use of a prescription binder called cholestyramine. Essentially, binders help to pull mycotoxins out of your body through your bowel movements.
- Antifungals: Itraconazole, voriconazole, and amphotericin B are prescription drugs that may be prescribed should you have a fungal infections. Some doctors also use natural antifungals like caprylic acid, thyme, oregano, or olive leaf.
- Immunomodulatory Nutrition Support: High doses of Omega-3 fatty acids or SPM’s (Specialized Pro Resolving Mediators) are frequently recommended to help support a healthy inflammation response.
- Targeted Supplements: Glutathione, NAC, alpha-lipoic acid, vitamin C, and probiotics are commonly recommended to support detoxification.
- Hyperbaric Oxygen Therapy (HBOT) – Commonly prescribed to reduce inflammation and enhance tissue oxygenation.
- Infrared Sauna – Commonly recommended to support detoxification through the sweat.
- Customized Nutritional Support – Many doctors measure for vitamin and mineral deficiencies. Based on test results, a customized nutritional protocol can be created that matches the needs of the patient.
Diet & Lifestyle Changes are Necessary to Recover
Unfortunately, this is an area many doctors fail to adequately address. Diet and lifestyle are too often an afterthought. I like to break this area down into 6 Essential Categories:
- Eat real, organic, whole foods – More on diet specifications below.
- Sleep – Sleep is essential for healing and repair. Chronic mold exposure causes insomnia for many, and sometimes getting sleep regulated again can be a challenge. Magnesium, melatonin, valerian, theanine, and passion flower can all be helpful if you are struggling.
- Exercise – The body needs movement to detoxify. Exercise can be tricky, as many mold sufferers don’t tolerate too much activity. The key here is to be patient with yourself. Move to tolerance. Walking small distances is a good place to start if that is all you are capable of.
- Sunshine – the freest and most powerful medicine on the planet is the sun. Go outside as much as you can. Aside from the fresh air, sunshine will provide a source of vitamin D, melatonin, serotonin, and stress hormone regulation. Additionally, sunshine helps your mitochondria generate more energy for healing and repair. Don’t underestimate how powerful sunshine is on your healing journey.
- Drink Clean Water – Your body is 70% water. Water is required to move toxins out of your body efficiently. Filter your water. Avoid drinking out of plastics. Use glass instead.
- Breath Clean Air – Now that your home is no longer a mold contaminated death box, your air quality should be much better when indoors. You should also consider an ultra fine HEPA filter as well. And did I mention – Go Outside! Even with filters, indoor air quality pails in comparison to mother nature.
Diet Changes Needed for Chronic Mold Exposure Recovery
The right dietary intervention is hands down, the most powerful tool when trying to recover from chronic mold exposure. Nutritional strategies help reduce inflammation, support detoxification, and minimize additional mycotoxin intake. In addition, nutrition is the cornerstone of healing. Your body requires adequate Calories (proteins, fats, & carbohydrates), vitamins, and minerals to heal, repair, and maintain itself. Without adequate nutrients, healing can at worst be impossible, and at best take longer than it should.
No Grain No Pain Diet
The No Grain No Pain diet is essential. Based on decades of clinical experience and patient outcomes, this diet often leads to rapid improvements for those with mold related illness. The core principles include:
- Eliminating Grains
- This includes wheat, corn, rice, oats, barley, and other cereal grains. Grains can contain elevated levels of mycotoxins, particularly when improperly stored or processed.
- By removing grains, many patients report a decrease in systemic inflammation, reduced joint pain, and an improvement in gastrointestinal symptoms.
- Focusing on Nutrient-Dense Foods
- Emphasize whole, unprocessed foods such as lean proteins, fresh vegetables, fruits (in moderation if blood sugar regulation is a concern), healthy fats (avocados, olives, coconut), and seeds or nuts that are low in mold risk.
- This ensures an abundance of vitamins, minerals, and antioxidants that support the immune system and aid in detoxification pathways.
- Avoiding Gluten and Cross-Reactive Proteins
- For many mold-affected individuals, gluten-containing grains can exacerbate leaky gut and inflammation—even if they do not have celiac disease.
- Identifying cross-reactive proteins (e.g., in certain grains or dairy) via testing or a structured elimination diet may further reduce immune system burden.
- Reducing Overall Inflammatory Load
- Chronic mold exposure can trigger a pro-inflammatory immune response. A diet devoid of grains (especially refined or genetically modified grains) often eliminates common inflammatory triggers, allowing the body to focus on healing and toxin elimination.
Avoiding High-Mycotoxin Foods
In addition to eliminating grains, a crucial strategy for mold recovery is minimizing dietary intake of foods known to contain high levels of mycotoxins:
- Peanuts and Peanut Products
- Frequently contaminated with aflatoxin, a potent carcinogenic mycotoxin.
- Opt for tree nuts like almonds or walnuts tested for mycotoxins, or choose peanut-free alternatives.
- Corn and Corn-Based Products
- Corn is prone to fumonisin and other mycotoxins if storage conditions are suboptimal.
- Check labels, as corn derivatives (corn starch, corn syrup) appear in many processed foods.
- Stored Grains and Cereals
- Wheat, barley, rice, and oats can be contaminated if not stored in dry, cool environments.
- Even on gluten-free diets, be mindful of how non-gluten grains (buckwheat, millet) are sourced and stored.
- Coffee and Certain Teas
- Improperly harvested or stored coffee beans can harbor mycotoxins such as ochratoxin A.
- Seek brands that test for mold contamination and maintain strict quality controls.
- Dried Fruits
- Figs, dates, raisins, and other dried fruits may develop fungal growth if moisture control is inadequate during processing or storage.
- Inspect for any visible mold and buy from reputable suppliers when possible.
- Cheeses and Fermented Products
- Some cheeses (especially soft varieties) and fermented foods (e.g., kombucha, miso) can be higher in molds.
- This does not mean all fermented foods are harmful, but individuals highly sensitive to mold or histamine may need to limit or temporarily avoid them.
Additional Considerations:
- Hydration and Electrolyte Balance
- Adequate fluid intake supports kidney and liver function, crucial for excreting toxins.
- Electrolytes (magnesium, potassium, sodium) maintain cellular and muscular health, especially important for those experiencing frequent urination or sweating due to mold-related issues.
- Testing for Food Sensitivities
- Chronic mold exposure overloads and sensitizes the immune system. A common side effect of this change is the development of food allergies and sensitivities. So in addition to removing grains and high-mold foods, patients may benefit from food sensitivity testing—particularly if symptoms persist despite dietary changes.
For more in depth information on this topic consider reading No Grain No Pain, and check out our Guide on Mold Detoxification.
Preventive Strategies & Maintenance
Mold can grow in as little as 48 hours. Once your mold is remediated, and your health is restored, it is important to implement a preventative strategy to ensure it doesn’t happen again.
- Perform Regular Visual Inspections: Keep your eyes open for signs of water intrusion or water damage.
- Immediate Response to Water Damage: Dry areas within 24 hours.
- Adequate Ventilation: Use exhaust fans in bathrooms/kitchens; maintain and clean HVAC systems regularly.
- Monitoring Indoor Humidity: Use hygrometers; aim for 30–50% humidity range.
For more detailed information, check out our Mold Prevention Guide.
FAQ: Common Questions About Mold Exposure and Toxicity
What is mold toxicity?
Mold toxicity occurs when a person is exposed to mold spores or mycotoxins (toxic substances produced by molds) for an extended period. This exposure can lead to various symptoms, chronic inflammation, the development of immune dysfunction, and even cancer.
What are the common symptoms of mold toxicity?
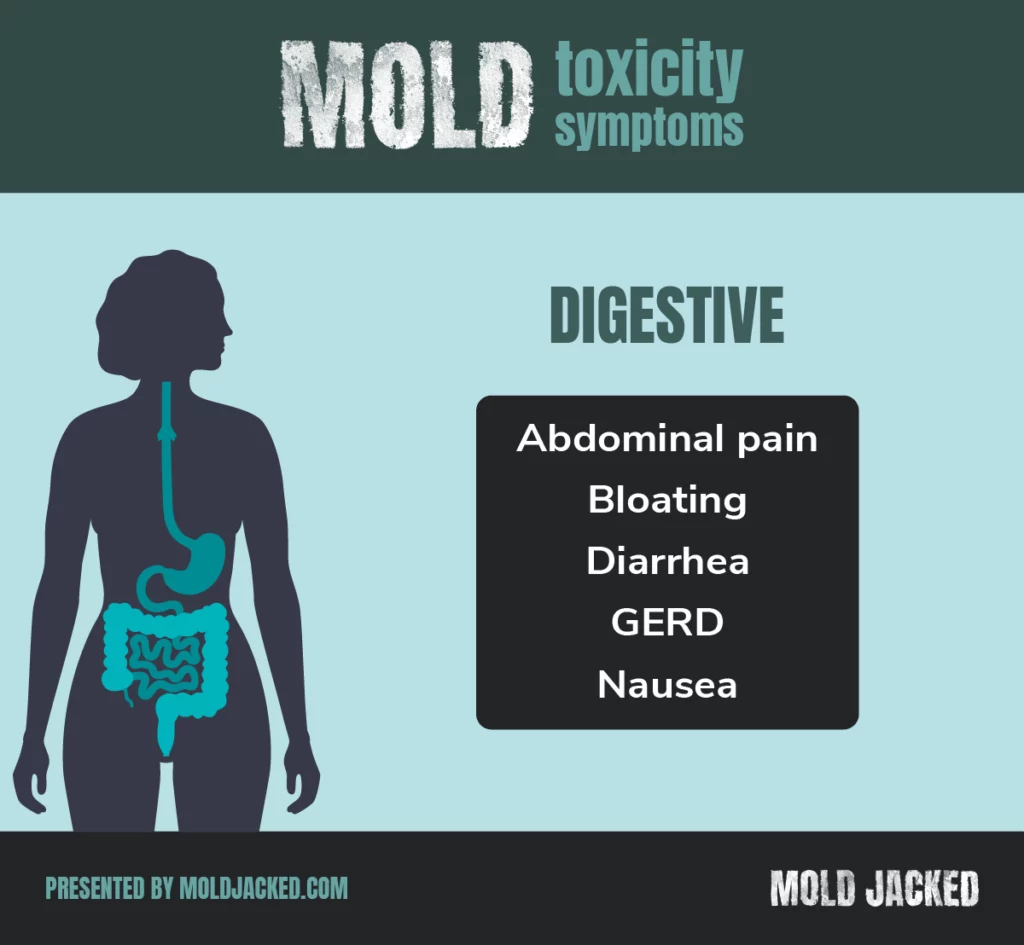
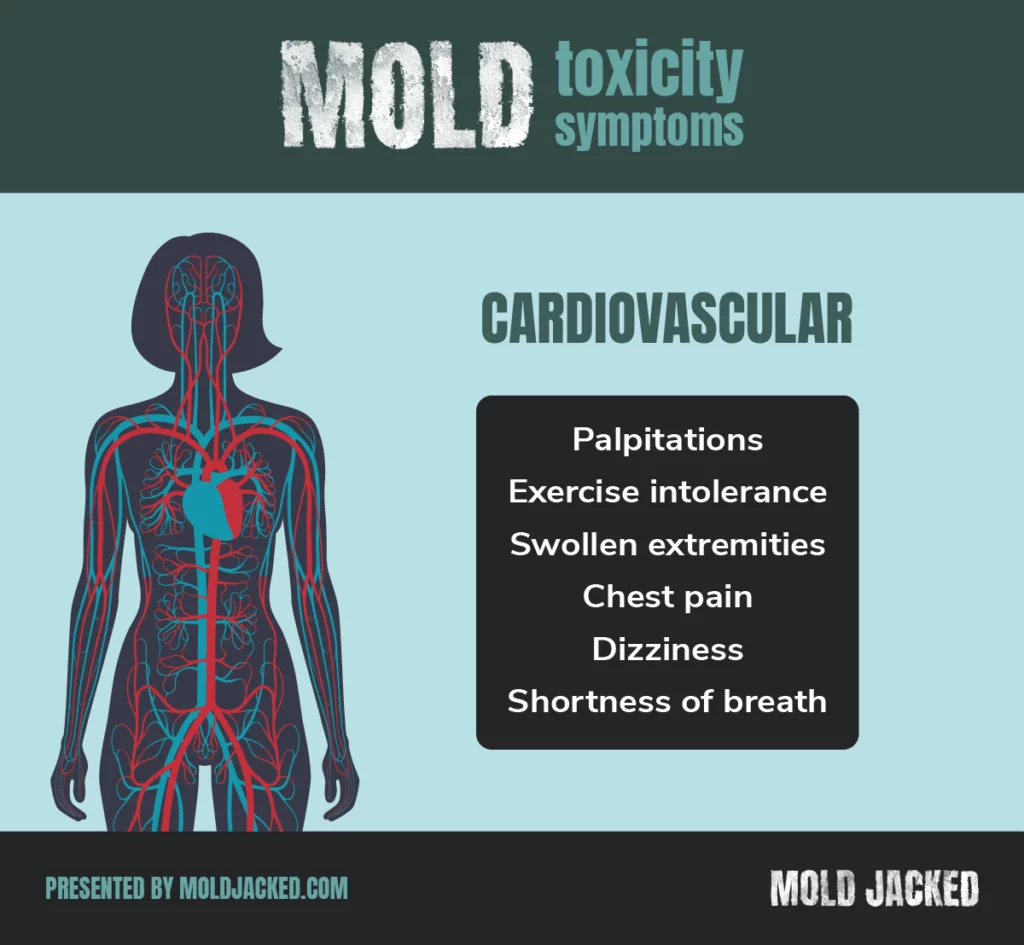
Symptoms of mold toxicity can vary but often include:
Chronic fatigue
Headaches and migraines
Difficulty concentrating or “brain fog”
Respiratory issues (coughing, wheezing, shortness of breath)
Skin rashes or irritation
Sinus congestion or sinusitis
Joint pain and muscle aches
Unexplained weight gain or loss
Digestive issues, including bloating, diarrhea, or constipation
Mood swings, anxiety, or depression
Can mold exposure alone cause cancer?
Yes. certain mycotoxins (aflatoxin B1) are strongly linked to liver cancer, and chronic mold exposure may contribute to tumor-promoting inflammation.
How do I differentiate mold toxicity from Lyme disease or co-infections?
Overlapping symptoms make it tricky; specialized testing for Lyme (Western Blot, PCR) and mycotoxins (urine panels) can help. Clinicians experienced in both conditions can provide a more holistic approach.
Can mold toxicity cause neurological symptoms?
Yes, mold toxicity is often linked to neurological symptoms, such as memory problems, confusion, and difficulty focusing. Individuals with mold exposure may also experience depression or anxiety, which can worsen the overall condition.
How can I tell if mold is affecting my health?
If you have a history of mold exposure and are experiencing unexplained symptoms, such as fatigue, respiratory issues, or cognitive problems, it’s important to consult a healthcare provider who specializes in mold toxicity. Testing for mold exposure or mycotoxins in your system can provide insight into whether mold is affecting your health.
Is mold toxicity the same as an allergy to mold?
Mold toxicity is different from a mold allergy. While an allergy triggers an immune response to mold spores, mold toxicity involves the buildup of toxic substances (mycotoxins) in the body. Both can cause similar symptoms, but mold toxicity tends to be more severe and long-lasting.
Can mold toxicity lead to chronic illness?
Yes, if left untreated, mold toxicity can contribute to chronic health conditions, such as Chronic Fatigue Syndrome (CFS), fibromyalgia, autoimmune diseases, and conditions like PANS (Pediatric Acute-onset Neuropsychiatric Syndrome).
What should I do if I think I have mold toxicity?
The first step is to minimize further mold exposure. Ensure your living or working environment is free from mold, and seek professional help to remediate any mold problems. Then, consult with a healthcare provider experienced in mold toxicity to evaluate your symptoms and recommend treatment options.
Are children more susceptible to mold toxicity?
Yes, children, especially those with underlying health conditions, are more vulnerable to the effects of mold exposure. Mold toxicity can also contribute to developmental or behavioral issues in children, so it’s essential to address mold problems in homes with young children.
Can mold toxicity be treated?
Yes, mold toxicity is treatable. Treatment often involves detoxification strategies, such as improving gut health, using binders to remove mycotoxins, and addressing any underlying inflammation. Your healthcare provider will tailor a treatment plan based on your specific symptoms and health history.
How can I prevent mold toxicity in my home?
To prevent mold growth, control moisture levels in your home. Repair leaks, use dehumidifiers, and ensure proper ventilation in damp areas like bathrooms and basements. Regularly check for mold growth and take action immediately if you spot it.
Is it enough to remove visible mold?
Not always. Hidden mold (behind walls, in HVAC) and mycotoxin-laden dust can perpetuate symptoms. A thorough inspection and remediation are critical.
Do I need to throw away all my belongings if I have mold?
Porous items (e.g., carpets, upholstered furniture) heavily contaminated with mold may need discarding. Non-porous or lightly contaminated items can often be cleaned with proper protocols.
Conclusion
Mold toxicity and mycotoxin exposure are multifaceted health issues that can involve respiratory, neurological, immunological, and even oncogenic (cancer-related) pathways. As research evolves, it becomes evident that mold-related illnesses aren’t solely about allergic responses but can encompass systemic inflammation, co-exposure synergies (e.g., heavy metals, food sensitivities, and genetic susceptibilities that compound the problem.
Effective diagnosis demands both clinical vigilance and specialized testing, while treatment combines environmental remediation, diet & lifestyle strategies, and sometimes medical interventions.
Ultimately, prevention through proper construction, proactive building maintenance, humidity control, and prompt water-damage remediation—remains the best defense against mold-induced illness.